When your immune system turns against your own body, things get complicated. Autoimmune diseases like Guillain-Barré syndrome, chronic inflammatory demyelinating polyneuropathy (CIDP), and immune thrombocytopenia don’t respond to simple fixes. That’s where IVIG therapy comes in - a treatment that uses antibodies from healthy donors to calm down a rogue immune system.
What Is IVIG Therapy?
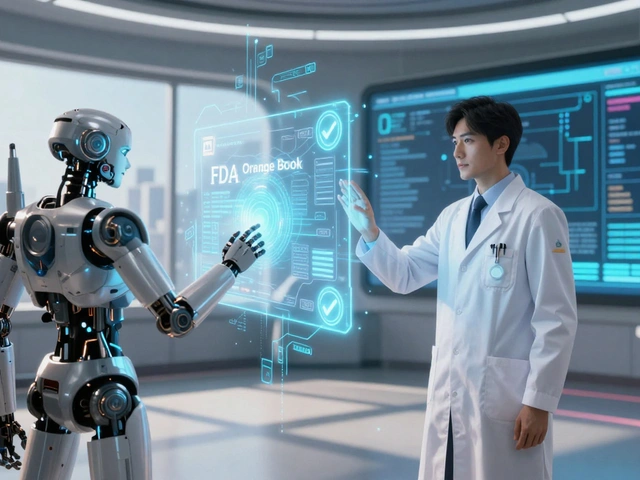
Intravenous immunoglobulin (IVIG) is a purified solution made from the plasma of thousands of healthy blood donors. It’s packed with immunoglobulin G (IgG) antibodies - the kind your body naturally makes to fight infections. But in IVIG, these antibodies aren’t meant to target germs. They’re used to reset your immune system when it’s attacking your nerves, muscles, or blood cells. It’s not new. Doctors started using IVIG in the 1950s to help people who couldn’t make their own antibodies. But by the 1980s, researchers noticed something unexpected: patients with autoimmune conditions like Kawasaki disease and immune thrombocytopenia started getting better. That’s when IVIG shifted from replacement therapy to immunomodulation. Today, IVIG is FDA-approved for several autoimmune conditions, including:- Kawasaki disease in children
- Immune thrombocytopenia (ITP)
- Guillain-Barré syndrome (GBS)
- Chronic inflammatory demyelinating polyneuropathy (CIDP)
- Dermatomyositis and polymyositis
How Does IVIG Actually Work?
It’s not just about adding antibodies. IVIG works in multiple ways at once:- It blocks harmful autoantibodies that attack your tissues
- It shuts down inflammatory signals like TNF-alpha and interleukins
- It prevents immune cells called macrophages from eating up your platelets or nerve cells
- It tweaks T-cells and B-cells to reduce overall immune activity
Who Gets IVIG Therapy?
IVIG isn’t for everyone. It’s typically reserved for specific situations:- Children with Kawasaki disease - given within 10 days of fever to prevent heart damage. Success rate? Around 95%.
- Adults with ITP who don’t respond to steroids or splenectomy - platelet counts jump in 24 to 48 hours.
- Patients with CIDP or GBS - IVIG is a first-line treatment. About 70% of CIDP patients see clear improvement.
- Pregnant women with autoimmune disorders - many drugs are off-limits during pregnancy, but IVIG is considered safe.
- People with refractory myositis - one trial showed 68% of patients gained at least 20% in muscle strength after IVIG.
What to Expect During Treatment
IVIG isn’t a quick pill. It’s an IV infusion that takes 3 to 6 hours per session. You’ll sit in a clinic, often in a recliner, while the solution drips slowly into your vein. The dose? Usually 1 to 2 grams per kilogram of body weight - so a 70 kg person might get 70 to 140 grams total. The infusion starts slow - about 0.5 mL per kg per hour - then speeds up if you tolerate it. Nurses watch for side effects. You’ll likely feel tired afterward. Some people get headaches, chills, or nausea. These are common - affecting 10-15% of infusions - but usually go away within a day. Serious reactions? Rare. Less than 0.5% of infusions cause kidney issues, blood clots, or severe allergic reactions. But if you have kidney disease or heart failure, your doctor will adjust the dose or slow the infusion. Most patients need repeat treatments. For CIDP or ITP, that’s often every 3 to 6 weeks. It’s a commitment. One study found 35% of CIDP patients quit IVIG because they couldn’t keep up with the time and travel.
How Fast Does It Work?
Speed is one of IVIG’s biggest advantages. Unlike methotrexate or mycophenolate - which can take months to work - IVIG often shows results in just 3 to 14 days. For ITP, platelets rise within 48 hours. In GBS, muscle strength improves within a week. That’s why it’s used in emergencies. But the effect doesn’t last forever. IVIG gets broken down by your body over time. That’s why maintenance doses are needed. The improvement is real - but temporary.Cost and Accessibility
IVIG is expensive. A single treatment cycle in the U.S. costs between $5,000 and $10,000. That’s because it takes plasma from thousands of donors to make one batch. Only four companies - Grifols, Takeda, CSL Behring, and Octapharma - control 85% of the global supply. Insurance usually covers it for FDA-approved uses. But prior authorizations are common. For off-label uses, you might need to fight for approval. There’s also a shortage risk. The global IVIG market hit $12.5 billion in 2023, and demand keeps rising - up 300% in the last decade. Autoimmune conditions are becoming more common, and doctors are using IVIG more often.IVIG vs. Other Treatments
How does IVIG stack up against alternatives?| Treatment | Onset of Action | Administration | Duration of Effect | Common Side Effects |
|---|---|---|---|---|
| IVIG | 3-14 days | IV infusion, clinic-based | 3-6 weeks | Headache, fatigue, chills |
| Plasma Exchange (PLEX) | 3-7 days | Specialized apheresis, clinic | 2-4 weeks | Blood pressure drops, tingling |
| Methotrexate | 6-12 weeks | Oral or injection | Long-term, daily | Liver toxicity, nausea |
| Rituximab | 4-8 weeks | IV infusion, every 6 months | 6-12 months | Infusion reactions, infection risk |
| Thrombopoietin Agonists (e.g., Romiplostim) | 1-2 weeks | Weekly injection | Long-term, daily use | Bone pain, headache |
What’s New in IVIG?
Research is moving fast. Scientists found that adding sialylated glycans to IVIG makes it 10 times more potent. That could mean lower doses and fewer side effects. Researchers at Rockefeller University have developed a synthetic version that’s 10 to 100 times stronger in animal models. If it works in humans, it could revolutionize treatment - less plasma needed, cheaper, more reliable. Combination therapy is also gaining ground. A 2024 review showed that IVIG + rituximab worked in 92% of severe autoimmune cases that didn’t respond to either drug alone. Subcutaneous IVIG (under the skin) is already available for some patients. It’s slower but lets people self-administer at home. That’s a game-changer for those who struggle with clinic visits.Real Patient Experiences
One woman with CIDP told her doctor she couldn’t walk without a cane. After two IVIG cycles, she walked into her next appointment without it. She’s been on maintenance every four weeks for three years. Her quality of life score improved by 50%. Another patient with ITP had platelets under 10,000. After IVIG, they jumped to 150,000 in two days. But the effect faded in three weeks. She now takes romiplostim injections between IVIG sessions. The biggest complaint? Time. A 4-hour infusion every month adds up. Many patients miss work or rearrange childcare. But for most, the trade-off is worth it.When IVIG Isn’t the Answer
IVIG isn’t magic. It doesn’t work for everyone. In Kawasaki disease, older children and boys are more likely to not respond. In GBS, older adults have worse outcomes. It’s also not first-line for every autoimmune disease. For example, it’s rarely used for lupus nephritis unless the patient is pregnant or has failed other treatments. And it’s not a cure. It’s a tool - one that buys time, reduces damage, and improves function. For many, it’s the difference between disability and daily life.What Comes Next?
The future of IVIG is about precision. Doctors are starting to monitor antibody levels after infusions to tailor dosing. Some centers are testing pharmacokinetic models to predict how long the treatment will last for each person. There’s also interest in using IVIG for long COVID autoimmune symptoms - a growing area of research. Early trials show promise in patients with persistent fatigue and nerve pain. The bottom line? IVIG therapy is one of the most powerful tools we have for autoimmune disorders. It’s not perfect. It’s not cheap. But for many, it’s the only thing that works.Is IVIG therapy safe for pregnant women?
Yes, IVIG is considered safe during pregnancy and is often used when other autoimmune treatments like methotrexate or biologics are contraindicated. It doesn’t cross the placenta in large amounts early in pregnancy and has been used successfully in conditions like immune thrombocytopenia and myasthenia gravis to protect both mother and baby. Studies show no increased risk of birth defects or complications when used under medical supervision.
How often do you need IVIG treatments?
It depends on the condition. For CIDP or chronic ITP, most patients get IVIG every 3 to 6 weeks. For acute conditions like Guillain-Barré syndrome, it’s usually a single 5-day course. Some patients with myositis may need monthly infusions for several months before switching to maintenance. The frequency is personalized based on how quickly your body breaks down the antibodies and how well your symptoms respond.
Can you get IVIG at home?
Yes - but only with a specific formulation called subcutaneous immunoglobulin (SCIg). It’s given under the skin over several hours, often using a portable pump. This option is available for patients with stable conditions who’ve tolerated IVIG well. Home administration reduces clinic visits and improves quality of life. However, not all insurance plans cover it, and it’s not suitable for acute or severe cases.
Why is IVIG so expensive?
IVIG is expensive because it’s made from human plasma collected from thousands of donors. Each batch requires extensive testing, viral inactivation, and purification to ensure safety. Only four major companies produce it globally, and manufacturing is complex and labor-intensive. The cost also includes clinical administration, nursing time, and monitoring. Insurance usually covers it for approved uses, but out-of-pocket costs can still be high without coverage.
What are the most common side effects of IVIG?
The most common side effects are mild and happen during or right after the infusion: headache (10-15%), chills (5-10%), nausea (5-10%), and fatigue (8-10%). These usually go away within 24 hours. More serious side effects - like kidney damage, blood clots, or severe allergic reactions - occur in less than 0.5% of infusions. Staying hydrated and slowing the infusion rate can help prevent most reactions.
Does IVIG weaken your immune system?
No, IVIG doesn’t weaken your immune system. It temporarily modulates it - calming down harmful activity without shutting it down. In fact, because it’s made from antibodies from healthy donors, it can even provide temporary protection against infections. However, people on long-term IVIG may still be at slightly higher risk for infections if their underlying disease affects immunity. It’s not immunosuppressive like steroids or biologics.




9 Comments
Erwin Kodiat
IVIG is one of those treatments that feels like magic until you see the bill. I’ve seen friends go through it for CIDP - the improvement is real, but the logistics? Brutal. Driving an hour, sitting for four hours, then crashing for a day. Worth it? Usually. But no one talks about how it eats into your life.
Christi Steinbeck
My sister got IVIG during her pregnancy for ITP - platelets were under 8k, and she was terrified. After the first infusion, she was holding our newborn like it was a normal day. No steroids. No scary meds. Just pure, donated antibodies doing their thing. It’s not perfect, but it’s a gift.
Josh Kenna
ivig is so expensive because its made from human plasma?? like… duh? but why are we still relying on donors? we have labs, we have tech, we have CRISPR. why are we still playing blood bingo with thousands of donors? this is 2024. we can make this synthetic. someone please tell the pharma giants to stop profiting off ancient methods.
Jacob Hill
I’ve been on IVIG for CIDP for five years now. Every four weeks. I used to hate it. Now I just schedule it like a dentist appointment. The fatigue? Yeah. The headaches? Always. But I walk. I drive. I play with my grandkids. That’s worth every penny, every hour, every needle prick.
Tracy Howard
Oh, sweet mercy - we’re still using this 1980s blood soup like it’s artisanal kombucha? In Canada, we’ve got better. We’ve got synthetic alternatives in Phase III. Meanwhile, Americans are still begging for plasma from truck stops and college kids. It’s embarrassing. The science is here. The will? Not so much.
Valerie DeLoach
For anyone thinking IVIG weakens immunity - it doesn’t. It’s like giving your immune system a gentle nudge to stop punching itself. The antibodies in IVIG are the same ones your body makes - just from someone else’s healthy system. It’s not suppression. It’s recalibration. And for pregnant women? It’s one of the safest tools we have. No teratogens. No fetal risk. Just quiet, powerful healing.
Lydia H.
I used to think IVIG was just a band-aid. Then I met a man with GBS who couldn’t lift his arm - and two weeks later, he was playing guitar again. It’s not a cure. But sometimes, healing doesn’t need to be permanent to be profound. Maybe the point isn’t to fix everything - just to give someone back their Tuesday morning.
Jackson Doughart
Subcutaneous IVIG changed my life. No more clinic. No more IVs. Just a small pump on my hip, overnight, while I sleep. I can travel. I can work. I can be normal. The downside? Insurance still fights it. But if you’ve tolerated IVIG well - push for SCIg. It’s not just convenient - it’s dignity.
Lewis Yeaple
While the clinical efficacy of IVIG in autoimmune conditions is well-documented, the pharmacokinetic variability among individuals remains a significant clinical challenge. The half-life of IgG is approximately 21 days, yet the duration of clinical benefit often diverges markedly from this parameter, suggesting that immune modulation - rather than mere antibody concentration - dictates therapeutic outcomes. Future personalized dosing regimens should incorporate FcRn receptor binding kinetics, IgG glycosylation profiles, and baseline autoantibody titers to optimize therapeutic windows and reduce cost burden. The emerging synthetic IVIG analogues, particularly those incorporating sialylated Fc domains, demonstrate not only enhanced anti-inflammatory potency but also reduced infusion-related adverse events - a critical advancement in translational immunology.