For patients taking medications like levothyroxine or phenytoin, a simple prescription refill shouldn’t turn into a weeks-long battle with insurance. Yet for those on NTI drugs - narrow therapeutic index medications - that’s exactly what happens. These drugs have such a small margin between the effective dose and the toxic one that even tiny changes in formulation can cause seizures, thyroid crashes, or worse. And yet, many insurers still force patients through prior authorization just to get the brand version, even when generics are available.
Why NTI Drugs Are Different
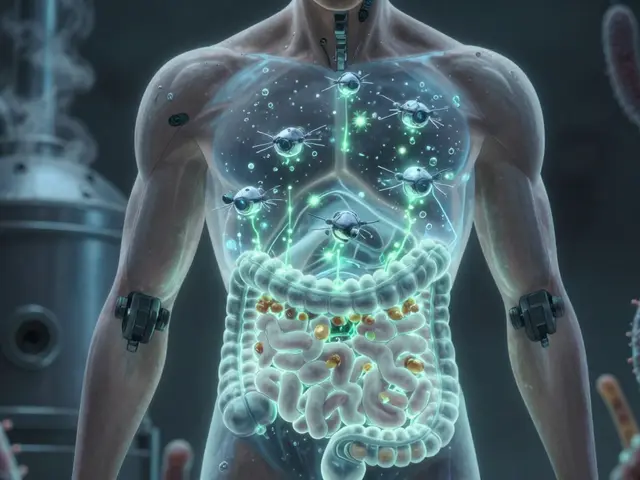
NTI drugs aren’t like regular prescriptions. A 10% change in blood concentration of levothyroxine can send a patient’s TSH levels soaring, leading to fatigue, weight gain, or heart problems. For epilepsy patients on carbamazepine or phenytoin, switching from brand to generic - or even between generic batches - can trigger seizures. The FDA defines NTI drugs as those where "small differences in dose or blood concentration may lead to serious therapeutic failures." There are about 37 of them on the market, including drugs for thyroid disorders, epilepsy, bipolar disorder, and blood thinning.Unlike most medications, where generics are bioequivalent and safe substitutes, NTI drugs are far more sensitive to manufacturing variations. A 2024 study in the Journal of Managed Care & Specialty Pharmacy found that 68% of patients on NTI drugs experienced delays in getting their prescribed brand medication, and 29% suffered direct health consequences - like hospitalizations or seizure spikes - because of those delays.
How Insurers Typically Handle NTI Drugs
Most insurance plans use prior authorization to block brand-name drugs when a cheaper generic exists. It’s a cost-control tool. But for NTI drugs, that logic breaks down. Some insurers, like Health Net, explicitly state that brand-name NTI drugs "may be listed on the Formulary at a higher tier and do not require prior approval." Others, however, still treat them like any other branded drug - requiring paperwork, doctor calls, and waiting periods.This inconsistency creates chaos. A patient in North Carolina might get immediate approval for brand levothyroxine, while someone in Texas gets denied and has to appeal. Medicaid programs are required by federal law to cover drugs excluded from formularies - but only if the patient goes through prior authorization. That means even government programs, meant to protect vulnerable populations, can delay life-sustaining meds.
Real Consequences: When Paperwork Kills
The human cost isn’t theoretical. A neurologist on Reddit shared that 73% of their levothyroxine brand requests were initially denied - even when patients’ TSH levels had swung 300% after switching to generics. One patient, after a 12-day delay getting their brand Keppra back, suffered a grand mal seizure. That’s not a rare story. The American Academy of Neurology’s 2024 study of 2,450 epilepsy patients found that unnecessary barriers to brand-name NTI antiepileptic drugs led to preventable seizures in 18.7% of cases.It’s not just epilepsy or thyroid patients. People on warfarin, digoxin, or cyclosporine face the same risk. A 2023 study showed that when prior authorization is required for NTI drugs, the average processing time is 3.2 business days. That’s over 72 hours without the exact medication their body depends on. And while 82.4% of denials are eventually overturned, that’s cold comfort to someone who’s had a seizure or gone into heart failure during the wait.
What Doctors and Pharmacies Are Up Against
Prescribers aren’t sitting idle. They’re spending hours filling out forms, faxing lab results, calling insurers, and resubmitting requests. A 2023 MGMA survey found that physicians spend an average of 16.3 hours per week just managing prior authorizations. That’s more than two full workdays - time taken away from patient care. And it’s not just paperwork. The required documentation is often excessive: weight, height, lab values, diagnosis codes, even prior treatment history. For NTI drugs, insurers demand even more - because they know the stakes are high.Electronic prior authorization systems have cut processing times by 42% overall, but NTI requests still take 22% longer than standard ones. Why? Because insurers demand extra clinical proof - even when the patient has been stable on the same brand for years. Some systems still require a new form for every refill, even if nothing has changed.
State Laws Are Starting to Change Things
Patients and doctors aren’t waiting for federal action. By June 2024, 22 states had passed laws limiting prior authorization for NTI drugs. California’s AB-1428, effective January 1, 2025, bans insurers from requiring prior authorization for NTI drugs if the patient was previously approved and their condition is stable. That’s a game-changer. It means if you’ve been on brand levothyroxine for six months and your labs are steady, your pharmacy should be able to refill it without a fight.Eighteen states now require automatic approval if the insurer doesn’t respond within a set timeframe - up from just seven in 2022. Some states mandate 24-hour reviews for urgent cases. Mississippi and North Carolina still require full prior authorization for most brand NTI drugs, but even there, pressure is mounting. The AMA’s 2024 State Law Chart shows a clear trend: lawmakers are recognizing that NTI drugs aren’t ordinary prescriptions.

What’s Coming Next
The federal government is catching up. The Improving Seniors’ Timely Access to Care Act, passed by the House in April 2024 with bipartisan support, will require Medicare Advantage plans to give real-time electronic decisions on prior authorization - including for NTI drugs. That means no more waiting days for a response. CMS has also started enforcing transparency rules, requiring insurers to publish their prior authorization criteria. Since that rule took effect, 37% more NTI drug requests are approved on the first try.Industry analysts predict that by 2026, 75% of commercial health plans will eliminate prior authorization for established NTI drug categories. The cost savings from avoiding hospitalizations and emergency care outweigh the small savings from switching to generics. And with 5.2% of all specialty drug prior authorizations now tied to NTI drugs - despite them making up only 2.8% of specialty drug use - insurers are realizing this isn’t sustainable.
What Patients Can Do Right Now
If you’re on an NTI drug and your insurer is giving you trouble:- Ask your doctor to write "medically necessary" or "brand required" on the prescription - some states require coverage if those words are present.
- Check your state’s laws. Many now have protections for NTI drugs - even if your insurer claims otherwise.
- Use electronic prior authorization portals when possible. They’re faster than fax or phone.
- Keep a log: note dates of denials, delays, and any health changes. This helps during appeals.
- If you’ve had a health event due to a delay, report it to Patients Rising or your state’s insurance commissioner. Data drives change.
You don’t have to accept delays. NTI drugs aren’t optional. They’re life-sustaining. And if your insurance is making you jump through hoops for a medication that could save your life - you’re not alone. More people are fighting back. And the rules are changing.
What are NTI drugs?
NTI drugs, or narrow therapeutic index drugs, are medications where even small changes in dosage or blood concentration can cause serious harm - like seizures, organ failure, or death. Examples include levothyroxine for hypothyroidism, phenytoin for epilepsy, and warfarin for blood thinning. The FDA defines them as drugs with a very narrow window between effective and toxic levels.
Why do insurers require prior authorization for NTI drugs?
Many insurers apply the same rules to NTI drugs as they do to other brand-name medications - trying to push patients toward cheaper generics to save money. But this ignores the medical reality: switching formulations can be dangerous. Some insurers still require prior authorization out of habit or outdated policy, even though major medical groups and state laws are pushing back.
Can I get a generic version of my NTI drug?
Technically, yes - many NTI drugs have FDA-approved generics. But the FDA and medical experts warn that these generics aren’t always interchangeable for NTI drugs. Even small differences in how the drug is absorbed can lead to dangerous fluctuations in blood levels. Many doctors and patients avoid generics for this reason. Some states now require a doctor’s note or prior authorization just to switch you to a generic.
How long does prior authorization for NTI drugs take?
On average, it takes 3.2 business days, but delays are common. Some insurers take over a week, especially if they request extra lab results or documentation. In urgent cases, federal Medicaid rules require a response within 24 hours and a 72-hour emergency supply. But commercial insurers often ignore those standards unless forced by state law.
What should I do if my prior authorization is denied?
Appeal immediately. Your doctor should submit a letter of medical necessity, including your diagnosis, lab results, and history of stability on the current medication. Many denials are overturned on appeal - 82.4% of them, according to one study. Also, check if your state has laws requiring automatic approval after a set time. If you’ve had a health issue because of the delay, report it to your state insurance commissioner or patient advocacy groups.
Are there any states that don’t require prior authorization for NTI drugs?
Yes. As of 2025, 22 states have passed laws limiting or eliminating prior authorization for NTI drugs. California, for example, now prohibits insurers from requiring prior authorization if the patient was previously approved and their condition is stable. Other states like New York, Illinois, and Washington have similar protections. Check your state’s health department website or the National Conference of State Legislatures for updated laws.




9 Comments
arun mehta
This is absolutely unacceptable. 🚨 I work in pharmacy in Bangalore, and I've seen patients cry because they couldn't get their brand levothyroxine for 11 days. One man had a seizure on Day 9. His TSH was 48. 🤯 Insurers think they're saving money, but they're just transferring the cost to ERs and ICUs. This isn't policy - it's cruelty dressed in bureaucracy.
Chiraghuddin Qureshi
Bro, in India we don’t even have access to generics for these drugs half the time 😅 But when we do, the batch variation is wild. One time my cousin’s phenytoin made her dizzy for a week - turned out the filler was different. So yeah, I get why docs won’t switch. But why do insurers act like we’re all just playing video games with our lives? 🤦♂️
Patrick Roth
Let me play devil’s advocate for a sec - if generics are FDA-approved, why are we treating NTI drugs like they’re magic unicorn pills? The data shows bioequivalence. Maybe it’s not the drug - maybe it’s bad adherence or poor lab monitoring. I’ve seen patients switch without issue. This whole thing feels like overmedicalized fear-mongering. 🤷♂️
Kenji Gaerlan
lol prior auth for thyroid med?? who even has time for this?? my guy just went 2 weeks without his pill and now he’s in the hospital. insurance company probably has 12 people just sitting around filing fax forms. i mean… why not just give people their meds??
Jasmine Bryant
I’m a nurse in Ohio and I’ve had to call insurers so many times for NTI drugs… I swear, half the reps don’t even know what NTI means. One time I had to send 7 lab results, a signed letter from the neurologist, and a copy of the patient’s 2022 MRI just to get them to approve a refill. It’s insane. And they still deny it. 😩
Sarvesh CK
It is worth reflecting upon the deeper philosophical implications of this systemic issue: when we reduce human health to a cost-benefit calculation, we erode the very foundation of medical ethics. The NTI drug dilemma is not merely administrative - it is existential. To deny a patient continuity of care for a life-sustaining medication, under the guise of fiscal prudence, is to commodify vulnerability. We must ask ourselves: what kind of society prioritizes balance sheets over brainwaves? The answer, unfortunately, is the one we live in - but change is not impossible. It begins with recognition, then advocacy, then legislation - and finally, compassion.
Hilary Miller
California’s law is a game-changer. If you’ve been stable? Just refill. No drama. 🙌
Brenda King
I’m a thyroid patient and I switched to generic once because my insurance forced it. I felt like I was drowning for 3 months. My heart raced. I couldn’t sleep. My doctor had to fight for 6 weeks to get me back on brand. Now I keep a printed copy of every denial in my file. If you’re going through this - you’re not crazy. It’s the system that’s broken. 💙
Keith Helm
While the human impact is undeniably significant, the economic burden on payers remains non-trivial. A wholesale elimination of prior authorization for NTI drugs may incentivize overutilization and undermine cost-containment strategies essential to long-term sustainability. A tiered, evidence-based exemption model - rather than blanket prohibition - is warranted.