Every year, thousands of people end up in the hospital not because their illness got worse, but because two of their medications clashed. It’s not rare. The average person over 65 takes nearly five prescription drugs. Add over-the-counter pills, vitamins, or herbal supplements, and the chances of a dangerous interaction jump dramatically. Generic drugs make up over 90% of prescriptions in the U.S., and while they’re cheaper, they’re not always easier to track. That’s where digital consultation tools come in - they’re not just convenient, they’re lifesaving.
Why Generic Drugs Are a Hidden Risk
People assume generics are just copies of brand-name drugs. They’re right - chemically, they’re identical. But here’s the catch: the same active ingredient can behave differently when mixed with other meds depending on the manufacturer’s fillers, coatings, or release mechanisms. A generic version of metoprolol from one company might interact with warfarin differently than another. Most patients don’t know this. Most doctors don’t either - unless they’re using a tool that flags it.Drug interaction databases don’t just look at the active ingredient. They track how each formulation affects absorption, metabolism, and excretion. That’s why checking for interactions isn’t enough anymore. You need to know which generic you’re prescribing - and how it plays with everything else.
What Digital Consultation Tools Actually Do
These aren’t fancy apps that just list side effects. They’re clinical decision engines. You type in a list of drugs - brand names, generics, even herbal supplements - and the system runs real-time analysis against thousands of known interactions. It doesn’t just say “possible interaction.” It tells you:- How severe it is (mild, moderate, severe)
- What’s happening in the body (e.g., one drug blocks liver enzymes that break down another)
- What to watch for (symptoms, lab changes)
- What alternatives exist
Some tools go further. UpToDate Lexidrug includes overdose treatment protocols - only one other platform does. Micromedex checks IV compatibility, which matters when a patient gets multiple drugs through an IV line. Epocrates lets you check up to 30 drugs at once. That’s critical for elderly patients on polypharmacy regimens.
Top Tools Used by Clinicians Today
Not all digital tools are built the same. Here’s what’s actually being used in clinics and hospitals right now:| Tool | Max Drugs Checked | Free Access | Overdose Info | EHR Integration | Best For |
|---|---|---|---|---|---|
| Epocrates | 30 | Yes (robust free tier) | No | Basic | Outpatient care, quick checks |
| Micromedex | Unlimited | No (paid only) | No | Advanced (hospital systems) | Hospitals, complex regimens |
| DrugBank | 5 | Limited (requires account) | No | None | Research, academic use |
| DDInter | 5 | Yes (no registration) | No | No | Academic research, open data |
| UpToDate Lexidrug | 50+ | No (subscription) | Yes | Partial | Clinical decision support, emergencies |
| mobilePDR | 10 | Yes (limited) | No | None | Official PDR data, quick reference |
Epocrates leads in outpatient settings because it’s fast, free, and lets you check a whole med list in seconds. Micromedex dominates hospitals because it ties into electronic health records, flags IV incompatibilities, and updates daily. For researchers, DDInter is the only open-access database built specifically for drug interactions - no paywalls, no sign-ups.
The Problem With Too Many Alerts
You’d think more warnings = safer care. But that’s not true. Clinicians are flooded with alerts. One study found doctors ignore between 49% and 96% of interaction warnings - not because they’re careless, but because so many are false positives.Take a common example: a patient on lisinopril (a blood pressure drug) and ibuprofen. The system flags an interaction. But if the patient only takes ibuprofen once a week for headaches, the risk is minimal. The tool doesn’t know that. It just sees two drugs.
That’s why top hospitals customize alert thresholds. They mute low-risk flags and only pop up severe ones. Without tuning, these tools become noise machines. And when you hear sirens all day, you stop listening.
How AI Is Changing the Game
The next wave isn’t just checking known interactions - it’s predicting new ones. In early 2024, DDInter released Version 2.0 with machine learning that spots patterns in unpublished data. Merative, the company behind Micromedex, bought a startup called InteracDx to do the same. Their goal? Cut false positives by 35%.The FDA now lists improved interaction algorithms as a priority. Why? Because over 1,500 new drug interactions are discovered every year. No human can keep up. But AI can scan millions of patient records, lab results, and drug trials to find hidden risks before they cause harm.
What You Should Do Right Now
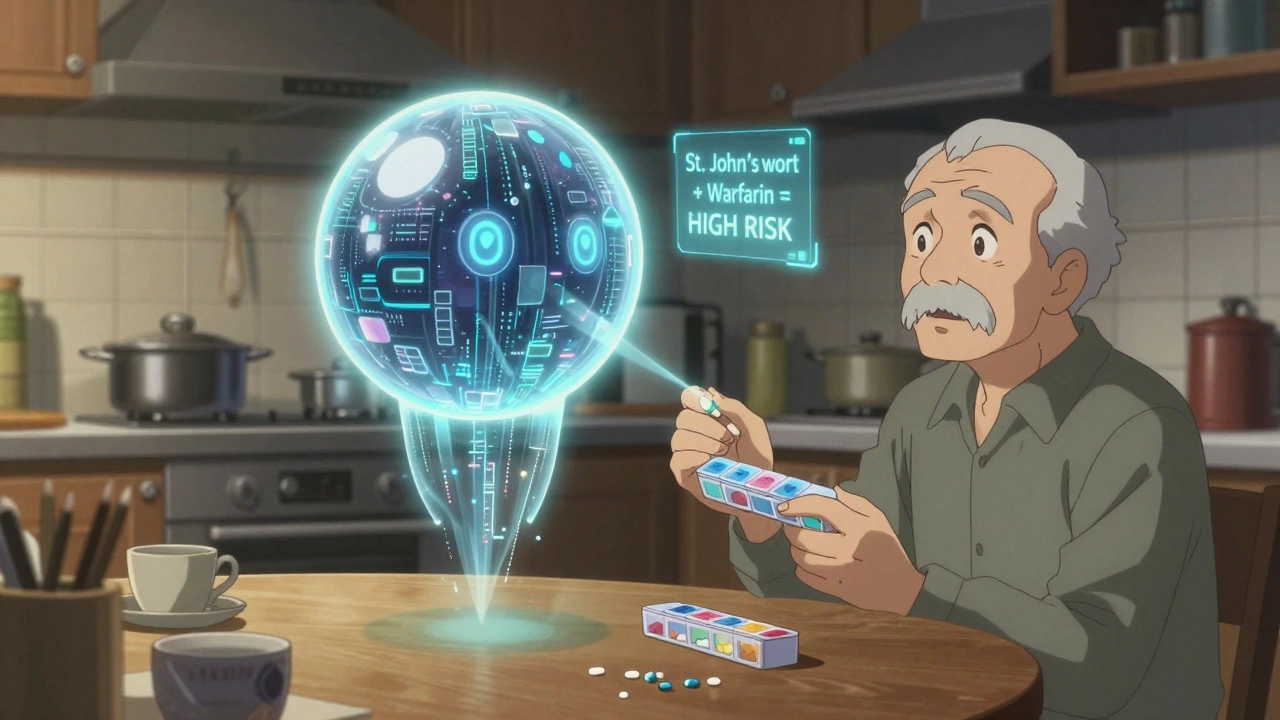
If you’re a patient: ask your pharmacist or doctor if they use a digital tool to check your meds. Don’t assume they’re doing it manually. Bring a full list - including supplements like St. John’s Wort or garlic pills. Those are often the culprits.If you’re a provider: test at least two tools. Try Epocrates for speed. Try Micromedex if you handle complex cases. Use DDInter if you’re researching. Don’t rely on one. No tool has all the data.
If you’re running an online pharmacy: integrate one of these tools into your prescription-checking workflow. It’s not optional anymore. The Joint Commission requires evidence-based clinical decision support for drug interactions. You’re legally expected to use them.
What’s Missing From Most Tools
Even the best tools have blind spots:- They rarely consider patient genetics - like CYP2D6 metabolism variations that make some people ultra-sensitive to certain drugs
- They don’t factor in kidney or liver function unless you manually enter it
- They miss interactions with medical devices - like how warfarin can react with certain pacemakers
- They don’t track timing - taking two drugs 12 hours apart might be safe, but the tool assumes simultaneous use
That’s why human judgment still matters. These tools are assistants, not replacements.
Real Impact: Numbers Don’t Lie
At Johns Hopkins Hospital, after implementing Epocrates and Micromedex across their system, preventable adverse drug events dropped by 27%. That’s not a small number. It means hundreds of patients avoided ER visits, hospitalizations, or worse.And it’s not just hospitals. In outpatient clinics using Epocrates, medication errors dropped by 19% in just six months, according to a 2023 AMA survey. These tools aren’t gimmicks. They’re proven safety nets.
Final Thought: It’s Not About Tech - It’s About Trust
The real challenge isn’t choosing the best app. It’s getting people to use it. Many doctors still open a printed drug guide. Many patients still don’t know their meds can fight each other.Technology won’t fix that. Education will. Start by asking: “Have you checked all these together?” Then show them the tool. Make it part of the conversation - not just a button you click.
Because in the end, a digital tool doesn’t save lives. People using it do.
Can generic drugs cause more interactions than brand-name drugs?
Not because of the active ingredient - generics are required to be bioequivalent. But differences in inactive ingredients (like fillers or coatings) can affect how quickly the drug is absorbed, which can change how it interacts with other medications. Some interaction tools don’t account for these subtle differences, which is why using a comprehensive system matters.
Are free drug interaction checkers reliable?
Yes - but with limits. Epocrates and DDInter offer free versions that cover most common interactions. But if you need to check more than five drugs, get detailed mechanisms, or access overdose protocols, you’ll need a paid tool. Free tools are good for quick checks, but not for complex cases. Always verify critical decisions with a pharmacist.
Do online pharmacies use these tools automatically?
Most reputable ones do - especially those tied to clinics or hospitals. But many small or international online pharmacies don’t. Always check if the pharmacy requires a prescription from a licensed provider and mentions clinical decision support. If they don’t, proceed with caution.
Can I use these tools to check my own meds?
You can - and you should. Epocrates has a free app that lets you enter your full med list. But don’t rely on it alone. Use it to prepare for your doctor visit. Bring the results and ask: “Is this safe with what I’m taking?” Never stop or change a drug based on an app alert.
Why do some tools only check 5 drugs at a time?
It’s a trade-off between accuracy and speed. The more drugs you add, the more complex the calculations become. Tools like DDInter and DrugBank were built for research and focus on detailed analysis of smaller combinations. Epocrates and UpToDate prioritize real-world use - they can handle 30+ drugs because they’re designed for busy clinics, not labs.
Are these tools regulated by the FDA?
No - not directly. But they’re held to clinical standards by organizations like The Joint Commission, which requires hospitals to use evidence-based tools. The FDA encourages their use and is pushing for better algorithms, but they don’t approve apps like they do drugs. That’s why it’s critical to choose tools backed by major medical institutions.




10 Comments
Scott van Haastrecht
This whole post is a glorified ad for corporate drug databases. Doctors don’t need another app-they need more time with patients. Every time I see one of these tools pop up, it’s another 30 seconds stolen from actual human interaction. And don’t get me started on how they flag every single combo as 'moderate risk'-half of them are noise. We’re drowning in alerts and dying of inattention.
Heidi Thomas
Epocrates is useless for anything beyond basic meds. If you’re managing polypharmacy in the elderly you’re either using Micromedex or you’re gambling with lives. No debate.
Rebecca Braatz
Hey everyone-just wanted to say this is such an important conversation. So many of us are taking 8+ meds and have no idea what’s happening under the hood. If you’re a patient, bring your full list to your pharmacist. They’ll thank you. If you’re a provider, don’t just click 'accept' on every alert-use these tools as conversation starters, not crutches. We’ve got this.
zac grant
Let’s not forget the CYP450 enzyme variability-genetic polymorphisms in CYP2D6, CYP3A4, CYP2C9 can turn a 'mild' interaction into a cardiac event. Most tools don’t integrate pharmacogenomic data unless you manually upload it. That’s a massive blind spot. We’re still treating patients like they’re all the same metabolic profile. We’re not.
Rachel Bonaparte
Oh wow, so now we’re trusting algorithms to decide who lives and who dies? How convenient. Let me guess-these tools are owned by Big Pharma subsidiaries? Of course they are. The same companies that invented the 'generic is just as good' myth while quietly changing fillers to extend patents. They don’t want you to know that a generic metoprolol from Teva might trigger a serotonin spike when mixed with fluoxetine, but a version from Mylan won’t-because the coating alters dissolution kinetics in the duodenum. And no, the FDA doesn’t require that data to be disclosed. So who’s really protecting you? The app? Or the corporate lawyers who own the database?
And let’s talk about UpToDate. Subscription-based. $2,000/year. Who’s paying for that? The hospital? The patient? Or are we just outsourcing clinical judgment to a paywall? Meanwhile, DDInter is open-source, built by researchers who actually care about public health. But nope-we’re all supposed to buy into the corporate wellness industrial complex. Classic.
And don’t even get me started on the 'AI predicting new interactions' hype. AI doesn’t discover anything. It correlates. And correlation isn’t causation. You think they’re training on real-world adverse event reports? No-they’re training on biased clinical trial data where the elderly, the poor, and the non-white are underrepresented. So the algorithm thinks 'no interaction' when it’s actually a death sentence for a 78-year-old with stage 3 CKD. Wake up.
These tools are digital placebos. They make us feel safe while the real problem-the lack of regulation, transparency, and accountability-grows louder. And the worst part? We’re being trained to trust machines more than our own instincts. And that’s not progress. That’s surrender.
Michael Feldstein
Really appreciate the breakdown on the tools. I’ve been using Epocrates for years in my clinic-fast, free, works great for quick checks. But I’ll admit, when I started seeing patients on 12+ meds, I switched to Micromedex for complex cases. The IV compatibility flag saved me once when a nurse was about to mix vancomycin with a dextrose bag. Would’ve precipitated. Scary stuff.
One thing I wish more tools did: allow you to tag meds as 'as needed' or 'occasional.' That way, the system knows ibuprofen once a week isn’t the same as daily. Would cut down on alert fatigue so much.
Carolyn Ford
Of course you’re recommending Epocrates-it’s free, it’s easy, it’s the lazy person’s drug checker. And you wonder why medication errors are still rampant? You’re not using the right tool because you don’t want to pay. Micromedex isn’t expensive-it’s essential. If you’re not using it, you’re not practicing medicine. You’re guessing. And guess what? Someone’s going to die because you didn’t upgrade your subscription.
jagdish kumar
Technology is the illusion of control. The real interaction is between fear and ignorance.
Ben Choy
I’ve seen firsthand how these tools change outcomes-especially in geriatric wards. One nurse told me she used to miss 3-4 interactions a week. Now, with Micromedex integrated into the EHR, she catches them before they happen. It’s not perfect, but it’s a lifeline. And yeah, the alerts are noisy-but you tune them. You don’t throw the baby out with the bathwater.
Also, big thanks to the author for mentioning DDInter. Open access matters. We need more of this.
Ollie Newland
Just came off a 12-hour shift at the VA. We had a 79-year-old on warfarin, amiodarone, and a new generic lisinopril. The tool flagged it as 'severe'-but the patient’s INR had been stable for months. Turns out, the new generic had a different filler that slowed absorption just enough to avoid the CYP2C9 inhibition. We didn’t change anything. The tool didn’t know that. The pharmacist did. Human + tool = safety. Not tool alone.
Also-yes, AI is coming. But until it can ask a patient, 'Do you take garlic pills?' or 'Does your daughter help you organize your pillbox?'-it’s just a fancy calculator.